Public Health Wales issues monkeypox guidance to control spread of disease as part of UK wide response
Public Health Wales has issued new monkeypox guidance to control the spread of the disease as part of the UK wide response to growing cases.
The UK Health Security Agency (UKHSA) have reiterated that the risk monkeypox poses to the UK public remains low.
As of 29 May, the total number of confirmed cases in England to 172, according to latest figures from UKHSA.
There are four confirmed cases in Scotland, two in Northern Ireland and one in Wales bringing the UK-wide total to 179.
The new guidance sets out measures for healthcare professionals and the public for managing the disease and preventing further transmission now that community transmission is occurring here in the UK and other countries.
People who have monkeypox can now isolate at home, if they remain well enough, whilst following measures advised in the new guidance to reduce further spread and while being monitored by local health protection teams.
In addition, UKHSA has purchased over 20,000 doses of a safe smallpox vaccine called Imvanex which is being offered to identified close contacts of those diagnosed with monkeypox to reduce the risk of symptomatic infection and severe illness.
The guidance published today recommends that:
People with monkeypox should avoid contact with other people until their lesions have healed and the scabs have dried off. Cases can reduce the risk of transmission by following standard cleaning and disinfection methods and washing their own clothing and bed linen with standard detergents in a washing machine.
Cases should also abstain from sex during the period of early symptom onset and avoid contact with any lesions. Whilst there is currently no available evidence of monkeypox in genital excretions, as a precaution, cases are advised to use condoms for 8 weeks after infection and this guidance will be updated as evidence emerges.
If people with suspected or confirmed monkeypox infection need to travel to seek healthcare, they should ensure any lesions are covered by clothing and wear a face covering and avoid public transport where possible.
Contacts of someone with monkeypox will also be risk assessed and told to isolate for 21 days if necessary.
Where possible, pregnant healthcare workers and severely immunosuppressed individuals should not assess or clinically care for individuals with suspected or confirmed monkeypox. This guidance will be reassessed as evidence emerges.
The minimum recommended personal protective equipment (PPE) for staff working with confirmed cases includes fit tested FFP3 respirators, aprons, eye protection and gloves.
For possible or probable cases minimum recommended PPE for staff includes fluid repellent surgical facemasks (FRSM), gowns, gloves and eye protection.
Within non-domestic residential settings (for example adult social care, prisons, homeless shelters, refuges), confirmed cases who are clinically well should be managed in a single room with separate toilet facilities where possible. Close contacts of these cases should be assessed for vaccination.
Dr Ruth Milton, Senior Medical Advisor and monkeypox Strategic Response Director, at UKHSA said:
This new monkeypox guidance sets out important measures for healthcare professionals and the public for managing the disease including how to safely isolate at home and reduce the risk to others.
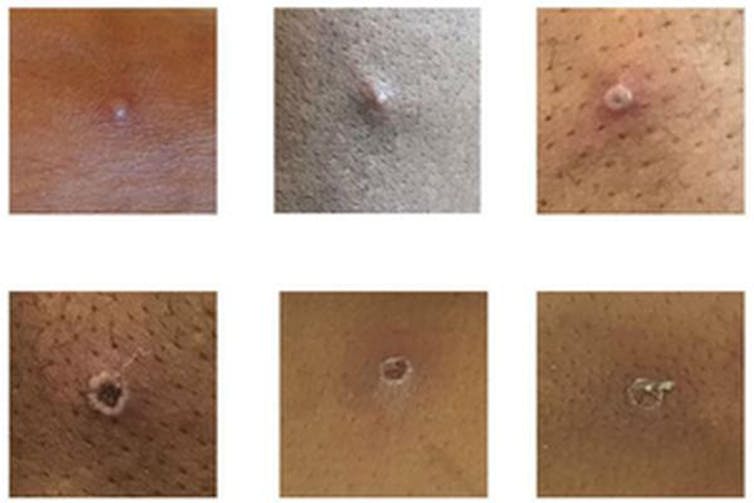
The highest risk of transmission is through direct contact with someone with monkeypox. The risk to the UK population remains low and anyone with unusual rashes or lesions on any part of their body should immediately contact NHS 111 or their local sexual health service.
Dr Giri Shankar, Director of Health Protection for Public Health Wales, said:
We are working with the UK Health Security Agency, Public Health Scotland, and Public Health Agency Northern Ireland to develop this guidance, which will ensure that healthcare staff in Wales have the best and most up-to-date knowledge on the management of Monkeypox cases.
We are reassuring people that monkeypox does not usually spread easily between people, and the overall risk to the general public is low. Anyone with unusual rashes or lesions on any part of their body should contact NHS 111 or call a sexual health service if they have concerns.
What are the symptoms?
Early symptoms are flu-like, such as a fever, headaches, aching muscles and swollen lymph nodes.
Once the fever breaks, a rash can develop, often beginning on the face and then spreading to other parts of the body – most commonly the palms of the hands and soles of the feet.
How deadly is monkeypox?
Monkeypox is mostly a mild, self-limiting disease lasting two-to-three weeks. However, in some cases, it can cause death. According to the WHO, the fatality rate “in recent times” has been around 3% to 6%. The west African monkeypox virus is considered to be milder than the central African one.
Monkeypox tends to cause more serious disease in people who are immunocompromised – such as those undergoing chemotherapy – and children. There have been no deaths from monkeypox in the current worldwide outbreak, but, according to the Daily Telegraph, one child in the UK is in intensive care with the disease.
Why is it called monkeypox?
Monkeypox was first identified in laboratory monkeys (macaques) in Denmark in 1958, hence the name. However, monkeys don’t seem to be the natural hosts of the virus. It is more commonly found in rats, mice and squirrels. The first case in humans was seen in the 1970s in the Democratic Republic of the Congo.
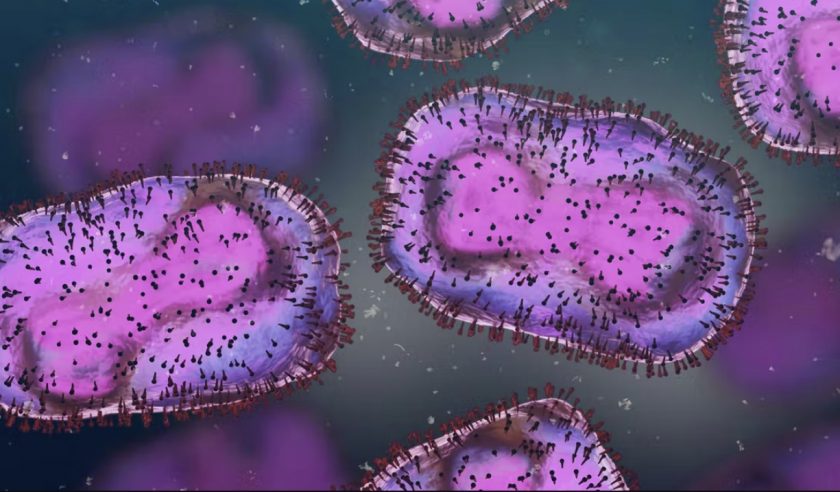
Is monkeypox related to smallpox and chickenpox?
Monkeypox is related to smallpox – they are both orthopoxviruses – but it is not related to chickenpox. Despite the name, chickenpox is a herpes virus, not a poxvirus. (How “chicken” got in the name is not entirely clear. In his dictionary of 1755, Samuel Johnson surmised that it is so named because it is “of no very great danger”.) Nevertheless, the vesicles (little pus-filled blisters) caused by monkeypox are similar in appearance to those of chickenpox.
Are cases likely to continue rising?
Cases are likely to continue to rise significantly over the next two-to-three weeks, but this is not another pandemic in the making. Monkeypox doesn’t spread anywhere near as easily as the airborne virus SARS-CoV-2 that causes COVID-19.
Has monkeypox evolved to be more virulent?
RNA viruses, such as SARS-CoV-2, don’t have the ability to check their genetic code for mistakes each time they replicate, so they tend to evolve faster. Monkeypox is a DNA virus, which does have the ability to check itself for genetic mistakes each time it replicates, so it tends to mutate a lot slower.
The first genome sequence of the current outbreak (from a patient in Portugal) suggests that the virus is very similar to the monkeypox strain that was circulating in 2018 and 2019 in the UK, Singapore and Israel. So it is unlikely that the current outbreak is the result of a mutated virus that is better at spreading.
How is monkeypox diagnosed?
In the UK, swab samples taken from the patient are sent to a specialist laboratory that handles rare pathogens, where a PCR test is run to confirm monkeypox. The UK Health Security Agency has only one rare and imported pathogens laboratory.
Is there a vaccine for it?
Vaccines for smallpox, which contain the lab-made vaccinia virus, can protect against monkeypox. However, the vaccine that was used to eradicate smallpox can have severe side-effects, killing around one in a million people vaccinated.
The only vaccine specifically approved for monkeypox, Imvanex, is made by a company called Bavarian Nordic. It uses a nonreplicating form of vaccinia, which causes fewer side-effects. It was approved by the US Food and Drug Administration and the European Medicines Agency in 2019 – but only for use in people 18 years of age or older.
UK health secretary Sajid Javid said that the UK government will be stocking up on vaccines that are effective against monkeypox. The UK currently has about 5,000 doses of smallpox vaccine, which has an efficacy of around 85% against monkeypox.
Are there drugs to treat it?
There are no specific drugs to treat monkeypox. However, antivirals such as cidofovir and brincidofovir have been proven to be effective against poxviruses in animals and may also be effective against monkeypox infections in humans.
[Image and Q&A republished from The Conversation under a Creative Commons license. Read the original article.]
Spotted something? Got a story? Send a Facebook Message | A direct message on Twitter | Email: [email protected]Latest News